Complex Trauma and the Brain
In Chicago and throughout the United States, the impact of complex trauma on our lives remains an often-overlooked issue. Here, we delve into the complex world of trauma – hoping to increase understanding of trauma and the multifaceted ways it manifests and affects the human brain.
By shedding light on the latest research findings, including the adaptive nature of trauma-induced brain changes and their potential long-term consequences, we hope to cultivate resilience, foster a greater understanding of complex trauma’s influence on Chicagoans’ daily lives, and appreciate the role trauma therapy can play in resolving trauma.
What is complex trauma?
The concept of complex trauma has evolved significantly over the past few decades. Initially, researchers and clinicians focused on single-incident traumas, like car accidents or natural disasters, and their psychological consequences. However, in the 1980s and 1990s, experts began understanding trauma better and recognized that some individuals experienced more pervasive, long-lasting effects resulting from ongoing or repeated trauma (especially when experienced during childhood or adolescence). This marked the beginning of our understanding of complex trauma and its far-reaching implications.
Complex trauma refers to a type of psychological trauma that typically arises from prolonged exposure to highly stressful and abusive situations. This can include experiences such as neglect, emotional, physical, or sexual abuse, domestic violence, or living in a highly unstable or chaotic environment. Unlike single-incident trauma, complex trauma involves multiple instances or a series of traumatic events that occur over an extended period, often at the hands of a caregiver or another trusted individual.
Complex trauma can have long-lasting effects on an individual’s mental, emotional, and physical health. It may result in difficulties with emotional regulation, attachment, trust, self-worth, and interpersonal relationships. Unfortunately, mental health disorders that can arise from complex trauma include complex post-traumatic stress disorder (C-PTSD), borderline personality disorder (BPD), anxiety disorders, and depression.
Understanding Trauma: Diagnosis and the Misdiagnosis of Trauma
Despite growing awareness, complex trauma remains challenging to identify and diagnose. A primary reason is that its symptoms can be easily confused with other mental health disorders, such as personality disorders, depression, and anxiety. Moreover, the subtle and pervasive nature of complex trauma means that many survivors (and therapists who aren’t well-trained in trauma therapy) may not even recognize their experiences as traumatic or attribute their struggles to those events. This lack of recognition can lead to delays in receiving appropriate support and treatment.
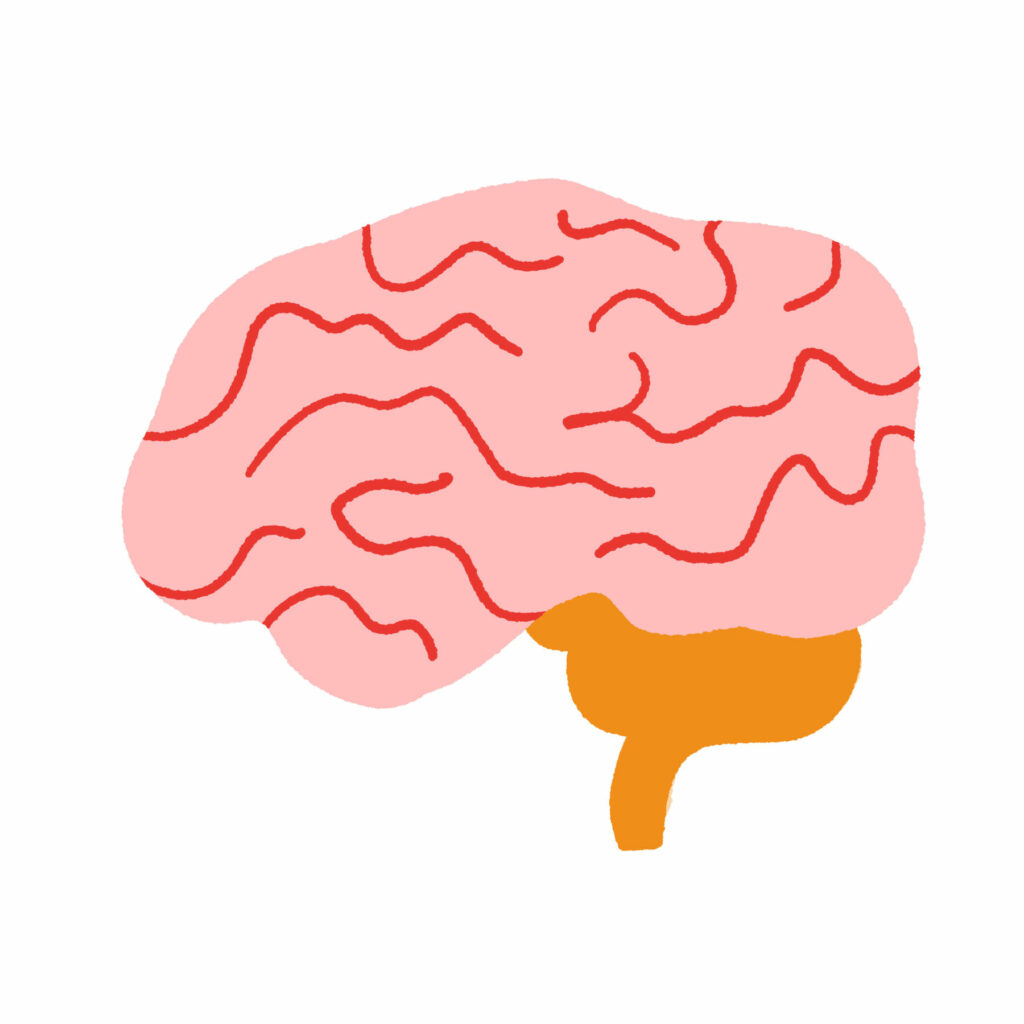
Complex Trauma’s Impact on the Brain:
Exposure to complex trauma during early childhood has been found to cause both structural and functional changes in the brain. Structural alterations involve changes in the size of specific brain areas, such as the enlargement of the amygdala (the brain’s alarm center) and the shrinking of the hippocampus (an essential region for processing and recalling traumatic experiences).
Functional changes, on the other hand, impact the activity of certain brain regions. This can lead to an overproduction of stress hormones in childhood, which may eventually weaken the immune system and result in the depletion of essential hormones required for tolerating and recovering from stressors in everyday adult life. A range of abnormalities, previously thought to be associated with psychiatric disorders, have been identified through neuroimaging and are now more accurately understood to be consequences of early childhood maltreatment.
Understanding Trauma and How It Impacts Brain Changes:
Because the brain changes as it grows through different development stages and because peoples’ capacity to cope changes with skill development, the timing of trauma can significantly influence the way the brain is impacted by complex trauma Some key factors are:
- Age: The brain undergoes significant development during childhood, particularly in the early years. Trauma experienced during critical periods of development may have more profound and long-lasting effects on brain structure and function, as the brain is more vulnerable and plastic during these times.
- Developmental milestones: Complex trauma occurring during crucial developmental milestones can disrupt the normal maturation of cognitive, emotional, and social skills, potentially leading to long-term deficits in these areas.
- Sensitive periods: There are specific windows of time during which the brain is particularly receptive to environmental influences. Trauma during these sensitive periods can result in more severe and lasting effects on brain development and functioning.
- Capacity for resilience: As individuals grow and mature, they develop coping mechanisms and resilience that can help them manage and recover from trauma. Experiencing complex trauma at a younger age, when these skills are not yet developed, can make it more difficult to process and overcome the traumatic event.
- Neuroplasticity: The brain’s ability to adapt and reorganize its neural pathways decreases with age. This means that the younger the individual is when experiencing trauma, the greater the potential for brain alterations due to the higher level of neuroplasticity.
- Cumulative effects: The impact of trauma on the brain can be cumulative, meaning that repeated or prolonged exposure to traumatic events may have more severe consequences than a single event. The timing of multiple traumas and the duration between events can also influence the overall impact on the brain (Hence, the development of symptoms of complex trauma.)
Are brain changes as a result of trauma adaptive?
Trauma-induced brain changes can be adaptive in some cases, as they serve to help individuals cope with and survive adverse experiences. Martin Teicher, a researcher at Harvard University, has extensively studied the effects of childhood trauma on brain development. According to Teicher’s work, some brain alterations resulting from trauma may provide a survival advantage in threatening environments. For example:
- Hypervigilance: Trauma can lead to enlargement of the amygdala, the brain’s alarm center. This change can result in heightened sensitivity to potential threats, allowing individuals to detect and respond to dangers more quickly. While this hypervigilance may be advantageous in hazardous environments, it can also contribute to anxiety and mood disorders in more stable settings.
- Stress response: Trauma can alter the stress response system, including the hypothalamic-pituitary-adrenal (HPA) axis. This may lead to the overproduction of stress hormones like cortisol, which helps the body mobilize resources in the face of a threat. However, prolonged exposure to stress hormones can have negative effects on physical and mental health, including a weakened immune system and an increased risk of depression.
- Memory processing: Trauma can cause changes in the hippocampus, a brain region involved in forming and retrieving memories. These changes may affect how traumatic memories are processed, potentially making it easier to suppress or dissociate from them, which can be adaptive in extreme situations. However, impaired memory processing can also lead to difficulties with emotional regulation and an increased risk of developing post-traumatic stress disorder (PTSD).
- Emotional regulation: Trauma can impact the prefrontal cortex, which is responsible for emotional regulation and decision-making. Alterations in this region may help individuals suppress strong emotional responses to trauma, allowing them to function in highly stressful situations. However, these changes can also lead to difficulties with emotional regulation, impulsivity, and an increased risk of substance abuse.
While these brain changes may provide short-term benefits in dangerous or threatening situations, they can lead to long-term negative consequences for mental and physical health when the individual is no longer in the traumatic environment. It is essential to recognize the adaptive nature of these changes and to develop targeted interventions that can help individuals who have experienced trauma to heal and adapt to healthier environments.
Can complex trauma be treated?
Treatment for complex trauma often involves a combination of therapeutic approaches, such as psychodynamic psychotherapy, cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and eye movement desensitization and reprocessing (EMDR). It is essential to work with trauma therapists who are experienced in treating complex trauma to ensure appropriate support and guidance throughout the recovery process
If this is the time to begin resolving your complex trauma, our trauma therapists would like to help. Contact us today!
This blog is made for informational and educational purposes only. It is not medical advice.
The information in this blog is not intended to (1) replace a one-on-one relationship with a qualified licensed health care provider, (2) create or establish a provider-patient relationship, or (3) create a duty for us to follow up with you.